Baby or not?

Treatment options have improved, and multiple sclerosis is often no obstacle to having children – as demonstrated not least by a nationwide register on the subject compiled by Professor Dr. Kerstin Hellwig. Here is an interview.
Published: 08.07.2025
Difficulty: intermediate
- Multiple sclerosis is often diagnosed at an age when women are thinking about starting a family. In the past, pregnancy was generally discouraged. Advances in treatment options now make it possible to fulfill the desire to have children.
- During pregnancy, the risk of a MS exacerbation decreases – even without medication. Affected women can lead a completely normal family life.
- As a precautionary measure, medications for multiple sclerosis are generally not intended for use during pregnancy. However, in animal experiments, only a few of these cause damage to the embryo.
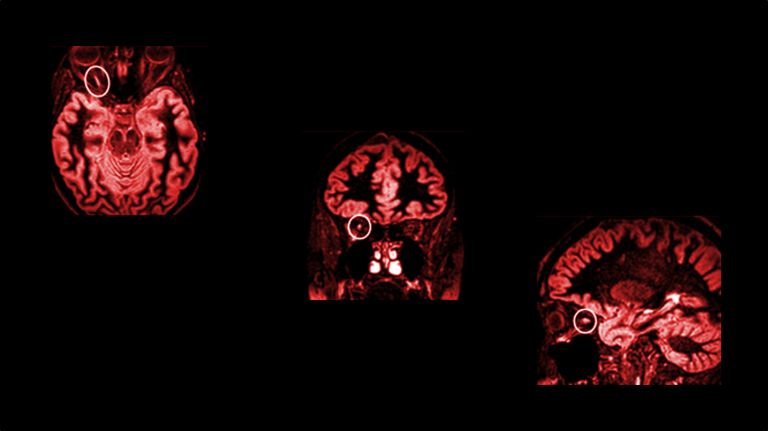
- Data on the effects on humans can only be obtained from a registry. In this registry, researchers systematically record existing pregnancies or attempts to become pregnant. Professor Dr. Kerstin Hellwig runs the world's largest registry of this kind at www.ms-und-kinderwunsch.de.
The German Multiple Sclerosis Society (DMSG) runs a nationwide project to provide advice on multiple sclerosis and the desire to have children. Contact persons at state level are available on a telephone hotline to answer all questions relating to the desire to have children, pregnancy, childbirth, breastfeeding, and parenthood. At the same time, regional network partners, such as MS centers and MS specialist doctor’s offices, are also involved. Kerstin Hellwig is also involved to ensure that medical questions are dealt with and answered appropriately. In addition, “Plan Baby with MS” is about establishing new networks and collaborations that enable and promote exchange betweenndividuals, regional network partners, and Kerstin Hellwig herself.
Director Rolf Schübel shot this film in 2003 with Franka Potente in the dual lead role. When Iris Sellin is diagnosed with multiple sclerosis, she has herself cloned so that her talent as a pianist is not lost. Her daughter Siri only finds out when she is 13 – and rebels. However, multiple sclerosis is never more than a hook for the story. At the center is the mother-daughter conflict over the self-realization of a wanted child, which could unfold almost exactly the same way without the extreme situation of cloning.
Recommended articles
Professor Hellwig, you maintain a nationwide registry on the topic of fertility in multiple sclerosis (MS). How did you come up with the idea of combining these two topics?
The diagnosis is usually made between the ages of twenty and forty. That's the age when people start thinking about having children. Otherwise, there is no obvious connection.
How did you come across this topic?
Hellwig: I was the only woman in the working group, and I was pregnant when we wanted to offer a workshop on pregnancy and multiple sclerosis. My (male) senior physician said at the time: “You do it.” And the participants had lots of questions that I couldn't answer. I thought I had prepared so poorly, so I researched everything again. It turned out that the data didn't exist. But I wanted answers. So, towards the end of my parental leave with my first child, I started running the registry. Then I went to the US, where I received training in clinical research and also found a job. Our registry at www.ms-und-kinderwunsch.de is now the largest in the world.
Is having children really the first thing that comes to mind for patients with multiple sclerosis? It's almost reminiscent of the plot of the film “Blueprint” (see box).
That's a bit extreme. Most of the women I deal with are like you and me. They work, then decide to start a family, and many want to return to work after one or two years of parental leave. They try to live a normal life. We now have such good treatment options, especially for relapsing MS, that at least remission can be achieved. But that still excludes pregnancy. I think that if we are so good at treating MS, at least relapsing MS, – then the issue of pregnancy must also be integrated. Typical cases tend to look like this: A couple has just returned from their honeymoon, is already planning a pregnancy or is even already pregnant, and then the first relapse occurs. How people deal with this varies greatly. It has to be discussed on a case-by-case basis. The tendency among doctors is to start MS medication first. But if the woman then becomes pregnant, the medication is usually discontinued. That's one advantage of pregnancy: the relapse rate usually decreases significantly. And if you only have to expect a relapse every two or three years, pregnancy is easy to plan. After the birth, however, we see an increase in relapses compared to the average before pregnancy. We currently know very little about how to manage this. But none of these issues are generally an obstacle. Multiple sclerosis is not a reason for me to advise against pregnancy. However, care should be taken to ensure that the disease is well controlled by MS therapy before actively planning a pregnancy.
In general, the risk of miscarriage is high in early pregnancy. Some activities are discouraged for expectant mothers in the first three months, partly because they might blame themselves in the event of a miscarriage. Are women with multiple sclerosis particularly susceptible?
Women with MS are no more at risk than healthy women. However, I have noticed that mothers with MS, at least those who contact me, often want to be particularly good mothers. This goes so far that at first, I thought: Help, the patients are all doctors! As if there were a particular occupational risk for MS. But these are simply the people who know that such a registry is the only way to obtain this kind of data, and so many women who are highly committed and well educated come forward. Fundamental uncertainties may still exist, however. Doctors and patients are extremely afraid of teratogenicity, i.e., anything that could cause malformations in the embryo.
Are there such problems with medications for multiple sclerosis?
The link between multiple sclerosis and pregnancy has only been studied for about twenty years. The drugs are still relatively new and must first be evaluated in terms of safety. It is only in the last twenty years that we have asked how safe it is to become pregnant while taking them. Due to the lack of data, at least in the beginning, warnings are included in the package insert, initially as a precautionary measure. Women should not become pregnant during clinical trials.
A few medications for multiple sclerosis are potentially harmful to the fetus – at least this has been observed in animal studies. Teriflunomide and cladribine are therefore contraindicated during pregnancy. A “Dear Doctor letter” has even been published for the S1P receptor modulator fingolimod: data collected after-market launch indicate an increased risk of congenital malformations, which is why its use is not recommended during pregnancy planning and pregnancy.
To be on the safe side, other S1P-receptor modulators such as ponesimod, siponimod, and ozanimod are also contraindicated during pregnancy.
In contrast, there is now very reassuring data on other MS drugs such as interferons, glatiramer acetate, dimethyl fumarate, ocrelizumab, and natalizumab. Experience with these substances is now available from over 500 pregnancies, and in the case of interferons and glatiramer acetate, even from over 2,500 pregnancies in which the last dose was taken shortly before or at the beginning of pregnancy. So far, these data show no evidence of teratogenic potential, which also opens up good treatment options for women with highly active disease before pregnancy.
Of course, pharmaceutical companies are not going to test their drugs on pregnant women from the outset.
In my opinion, the fact that there has been so little data for so long is also due to the fact that more men than women were involved in research in the past. The collection of pregnancy data is, of course, more of a women's research topic. I would like to know things like: How many out of a hundred women experience a severe flare-up when they stop taking the medication? How safe is breastfeeding while taking medication? And much more. We are now well on the way – not only through international cooperation, but also through our own extensive data collection and the willingness of patients to participate. Nevertheless, more information is still needed, especially for the newer drugs, in order to be able to give even better recommendations. Long-term follow-up studies of pregnancies are currently lacking, which is why we monitor the children of our study participants until they reach the age of 6.
Is that one of the goals of your registry? What can be learned from collecting data on pregnancies or fertility treatments in women with MS?
We want to find out what the best treatment options are for the mother without harming the child. I see it as my main task to find the best balance so that pregnancy does not cause any problems for the mother but also ensures the safety of the child.
You are now even researching how artificial insemination is compatible with multiple sclerosis.
The latest studies show that the risk of relapses is not increased after reproductive medical treatments. All hormones can be administered. The risk of a relapse is even lower if MS therapy is continued during treatment.
Thank you very much.
Further reading
- German-language Multiple Sclerosis and Fertility Registry (DMSKW); URL: http://www.ms-und-kinderwunsch.de [as of June 8, 2025]
First published on May 30, 2017
Last updated on July 8, 2025