Legalize it?! What are the medical benefits of cannabis?

Cannabis has been around for a long time. Even though many swear by substances containing cannabinoids, their medical benefits are the subject of controversy among experts.
Scientific support: Prof. Dr. Dieter K. Meyer, Prof. Dr. Rainer Spanagel
Published: 11.12.2025
Difficulty: intermediate
- The hemp plant has been around for a long time, including as a remedy. The 2017 German Cannabis Act added cannabis-based preparations to the list of services covered by health insurance companies, thereby facilitating their legal use. However, not all medical professionals are happy about this.
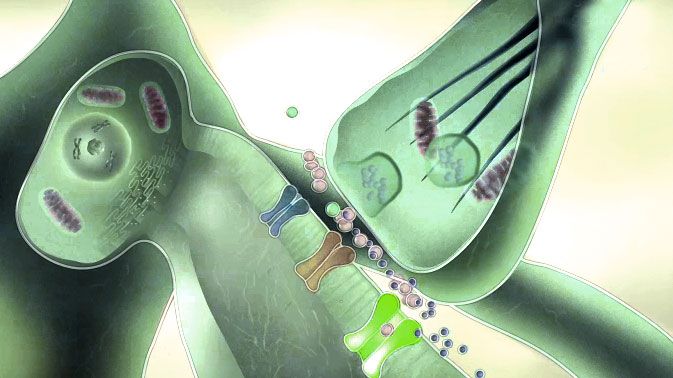
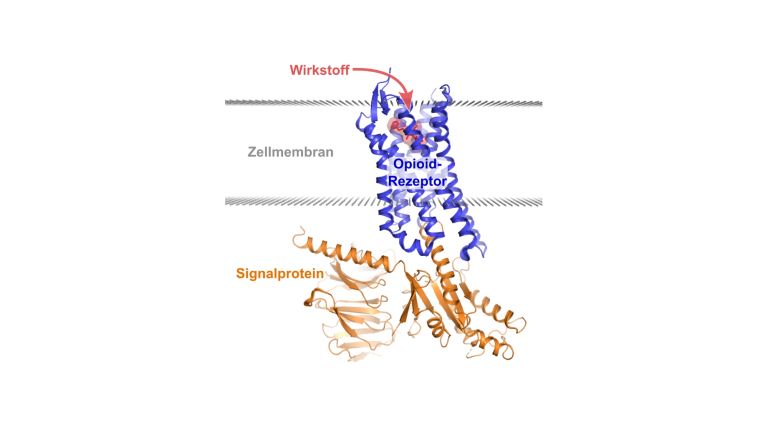
- Active ingredients from the hemp plant, such as THC or CBD, bind to the cannabinoid receptors CB1 and CB2 in the body. The body's own messenger substances that activate these binding sites are called endocannabinoids. Together, they form the endocannabinoid system.
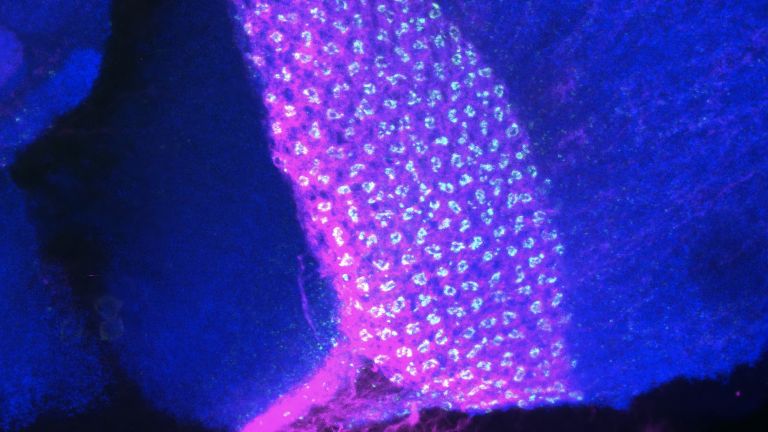
- The endocannabinoid system (ECS) is well characterized – it influences our emotional behavior, motivation, and cognitive processes. The ECS is also involved in a variety of physiological processes. These include, for example, immune function, appetite regulation, and pain perception. It also plays an important role in the development of the nervous system.
- Doctors may prescribe cannabis-based medications if other preparations have not been sufficiently effective or if suitable alternatives are not available. This gives them a great margin of discretion.
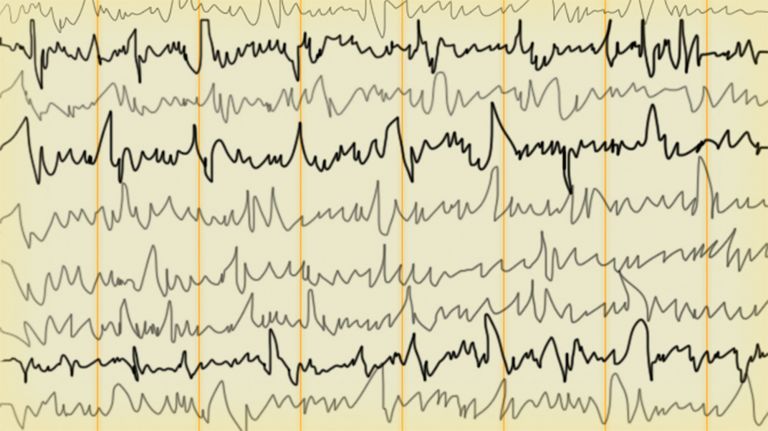
- Clinical studies indicate the effectiveness of cannabis preparations in treating certain conditions such as chronic pain. CBD is approved as Epidolex and is highly effective in treating childhood epilepsies such as Lennox-Gastaut syndrome and Dravet syndrome. However, its additional benefits in treating many other conditions remain controversial, even among experts.
- Acute side effects of cannabis-containing preparations include fatigue, dizziness, or euphoria, but anxiety or panic can also occur. Less is known about the long-term effects, but there is evidence of reduced cognitive abilities and an increased risk of mental illness in susceptible individuals. In particular, the risk of psychosis increases significantly with the use of high-dose cannabis products. Because the endocannabinoid system plays a role in the development of the nervous system, experts warn young people in particular against reckless consumption. Cognitive abilities can be permanently impaired by high cannabis consumption in adolescence.
- Further controlled studies are needed to better understand the full profile of cannabis-based products. This should also include better research into the biological mechanisms of THC and CBD.
The hemp plant and its extracts have been used by humans for a long time. In many ancient cultures, cannabis has been used for medicinal and ritual purposes for thousands of years. In Europe, it was widely used for therapeutic purposes as early as the 19th century, for example in the treatment of pain. After that, however, the hemp plant and its medicinal use fell into oblivion in the West – though not necessarily its “non-therapeutic” effects – from which the hemp plant and its extracts seem to be slowly reawakening. Among experts, however, its medicinal benefits are anything but undisputed.
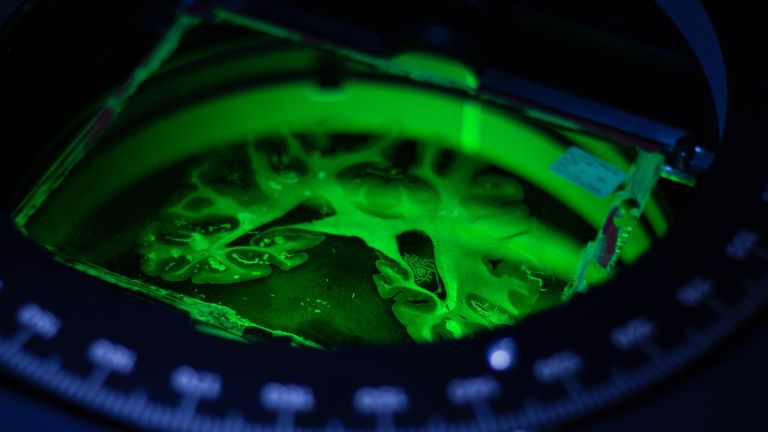
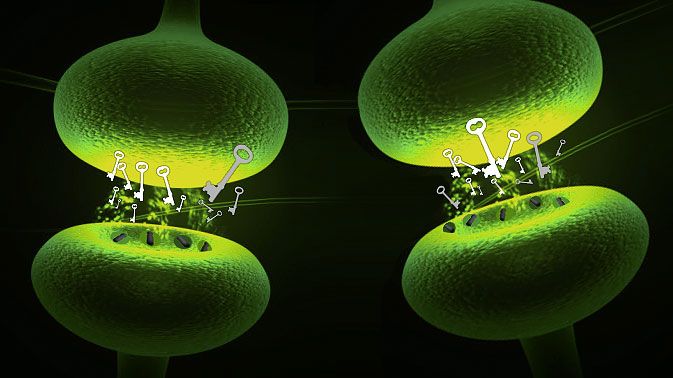
It was not so long ago that the biological cause of the diverse effects of cannabinoids was deciphered. Around 1990, it was discovered that the psychoactive substance tetrahydrocannabinol, or more precisely 9-tetrahydrocannabinol – better known as THC or dronabinol, the international nonproprietary name – binds to specific cannabinoid receptors in the brain. Since it seemed implausible that evolution would produce a lock in the brain specifically for a key that can only be found in the hemp plant, the search began for the body's own binding partners, the “endogenous cannabinoids.” The first such substance to be isolated was anandamide, derived from the Sanskrit word for “inner delight,” which was isolated from pig brains in 1992. We now know that the endocannabinoid system consists of two different cannabinoid receptors (CB1 and CB2). These are scattered throughout the central and peripheral nervous systems and influence important physical processes such as immune function, appetite regulation, memory, and pain perception. The endocannabinoid system also plays an important role in the development of the nervous system and in adolescence. For example, there are significantly more CB1 receptors during adolescence than in adulthood.
However, THC is not the only active ingredient in the hemp plant. Another (less conspicuous) substance is cannabidiol (CBD). It also exerts its effect via cannabinoid receptors, but often with effects opposite to those of THC. CBD is not psychoactive and does not make you “high” – which is why, unlike THC, CBD is not subject to the German Narcotics Act (BtMG). Its antispasmodic effect in childhood epilepsy is well documented and is used in clinical applications. Whether CBD has anti-inflammatory and antipsychotic effects is still not conclusively clear.
THC: Old wine in new bottles?
The oral spray Nabiximols (trade name Sativex) was the first cannabis-based drug to be approved in Germany in 2011. It contains a standardized cannabis extract of THC and CBD in a 1:1 ratio and is intended for the treatment of spastic symptoms in patients with multiple sclerosis. Since then, another cannabis-based active ingredient, nabilone (trade name Canemes), has been approved. Until March 10, 2017, however, the prescription of cannabis-based medications was made difficult by the fact that health insurance companies were allowed to refuse to cover the costs. Although German doctors were able to prescribe preparations such as Sativex as part of an individual therapeutic trial, there was a risk that patients would be left to bear the costs themselves. With the so-called Cannabis Act, the coverage of treatment costs was included in the health insurance companies' catalog of services. For many doctors, however, this raises more questions than answers.
Medications containing cannabinoids are generally intended for patients for whom conventional therapies are not sufficiently effective. However, the law gives doctors a great deal of discretion in this area, as it does not provide any direct guidelines on approved indications. It is therefore left to the physician to decide where “a generally recognized service that meets medical standards is not available in individual cases” or “in individual cases, according to the justified assessment of the treating contract physician, cannot be used after weighing the expected side effects and taking into account the insured person's medical condition,” as the legislator puts it. Controlled studies have found evidence of the efficacy of dronabinol, particularly in the treatment of spasticity (e.g., in multiple sclerosis), loss of appetite and nausea (e.g., during chemotherapy), and chronic pain (e.g., in rheumatism). However, it should not be forgotten that the data is still quite uncertain, partly due to a lack of or suboptimal clinical studies.
In 2025, a well-controlled Phase III study on a cannabis extract and its effectiveness in chronic back pain was published for the first time. This study could soon lead to European approval – 450 million people worldwide suffer from chronic back pain. Until now, treatment has mainly involved opiates – which has also contributed to the American opioid crisis. According to the Centers for Disease Control and Prevention (CDC), over 500,000 deaths due to opioid overdoses have been recorded in recent years. A cannabis extract would be a blessing as an alternative here.
Recommended articles
Time for fundamental approval?
Regardless of their therapeutic effectiveness, cannabinoid-containing drugs are not harmless. The most common acute side effects include fatigue, dizziness, palpitations, and increased appetite. In addition, THC in particular triggers psychological effects such as euphoria, altered perception, and relaxation – but anxiety and panic can also occur. Much depends on the THC to CBD ratio, which has shifted in favor of THC in recent years' strains. The cannabis of the hippie movement of the 1960s is therefore only comparable to today's cannabis to a limited extent. Over the past 50 years, the THC content has increased almost tenfold. This is worrying because higher THC content also greatly increases the risk of psychosis.
Cannabis-containing preparations can also lead to impaired memory and motor skills, which affects driving ability. Since the endocannabinoid system plays an important role in the development of the nervous system, cannabis use can pose serious risks, especially for young people.
Animal experiments have shown that the long-term effects of cannabis compounds cause serious and permanent impairments. In humans, longitudinal studies over a lifetime are extremely costly, so there are few reliable findings. Permanent impairment of cognitive performance after very high doses is possible. Withdrawal symptoms, as described with other drugs, appear to be a rare problem when used correctly for medical purposes. However, the extent to which cannabis preparations are a “gateway drug” to other substances (gateway hypothesis) remains a subject of controversy. Current research suggests that the relationship between cannabis use and the use of other drugs such as cocaine cannot be viewed in a one-dimensional way – the context of broader social and individual variables plays a decisive role here. From the point of view of many researchers, the gateway hypothesis should therefore not be used politically as an argument against cannabis use.
Cannabis-based medicines certainly have potential in the treatment of certain diseases. However, further clinical studies that meet high methodological standards are needed to substantiate such assumptions. Above all, this should be done without reservation for the benefit of patients – by both proponents and opponents.
First published on April 5, 2018
Last updated on December 11, 2025